Cardiac Cycle: Anatomy and Physiology
Estimated reading time: 11 minutes
The Cardiac Cycle is everything that happens in the heart from one beat to the next. The heart’s rooms tighten and relax in a pattern. This helps blood flow well.
The cardiac cycle: a rhythmic dance of life, a testament to the heart’s enduring power.
Here’s a breakdown of the key phases:
- Systole (Contraction):
- This is the phase when there are heart muscle contractions, pumping blood out of the chambers.
- So, first, the upper heart chambers squeeze. Then the lower heart chambers squeeze.
- Diastole (Relaxation):
- This is the phase when the heart muscle relaxes, allowing the chambers to fill with blood.
- Also, it involves the relaxation of their atria and ventricles.
The Cardiac Cycle can be further divided into more detailed stages, including:
- Atrial Systole:
- The atria contract, pushing blood into the ventricles.
- Ventricular Systole:
- The heart’s rooms also tighten. Blood goes into the aorta. The aorta takes blood away from the heart’s left side. Also, blood goes into the pulmonary artery. This artery takes blood away from the heart’s right side.
- Ventricular Diastole:
- Even the ventricles relax, allowing them to fill with blood from the atria.
- Atrial Diastole:
- Thus, the atria relax, and blood returns from the veins.
In essence, the Cardiac Cycle is a continuous process of contraction and relaxation that ensures a constant flow of blood.
Phases of the Cardiac Cycle
The heart’s cycle has different parts. Also, each part is important for the heart to pump blood well. Here is a close look:
1. Atrial Systole:
- The atria contract, pushing the remaining blood into the ventricles.
- Also, this completes the filling of the ventricles.
2. Ventricular Systole (Contraction):
- This phase is further divided into:
- Isovolumetric Contraction:
- The ventricles begin to contract, but both the atrioventricular (AV) and semilunar valves are closed.
- Also, this causes a rapid increase in ventricular pressure.
- Ventricular Ejection:
- When the heart’s bottom sections push harder than the big blood tubes, the flaps open. This lets blood move ahead. Blood then exits the lower heart areas and enters the arteries.
- Isovolumetric Contraction:
3. Ventricular Diastole (Relaxation):
- This phase is also divided into:
- Isovolumetric Relaxation:
- The ventricles relax, and the semilunar valves close.
- Specifically, all valves are closed, and thus, ventricular pressure decreases.
- Isovolumetric Relaxation:
4. Atrial Diastole:
- While the ventricles are filling, the atria are also relaxing.
- Also, this allows blood to flow back into the atria from the veins.
Key points to remember:
- Systole: Contraction
- Diastole: Relaxation
Thus, the opening and closing of heart valves are driven by pressure changes within the heart chambers.
How Does Each Phase Contribute to Heart Function
- Atrial Systole:
- Completes ventricular filling, ensuring maximum blood volume before ventricular contraction.
- This “atrial kick” is especially important during rapid heart rates.
- Ventricular Systole (Isovolumetric Contraction & Ventricular Ejection):
- Additionally, isovolumetric contraction builds pressure within the ventricles, preparing for forceful ejection.
- Also, when the heart’s lower chambers pump, oxygen-rich blood goes from the left side to the body. At the same time, blood without much oxygen goes from the right side to the lungs.
- Moreover, this is the phase that provides the bodies blood supply.
- Ventricular Diastole (Isovolumetric Relaxation & Ventricular Filling):
- Thus, isovolumetric relaxation allows ventricular pressure to drop, even enabling the AV valves to open.
- Also, ventricular filling allows the ventricles to refill with blood, preparing for the next contraction.
- Moreover, this is the phase that allows the heart to refill with blood.
- Atrial Diastole:
- Allows the atria to receive blood from the veins, also ensuring a continuous flow of blood into the heart.
What Role Do Valves Play in the Cardiac Cycle
Heart valves are essential for maintaining unidirectional blood flow through the heart. Also, they ensure that blood moves forward and prevent backflow. Here’s their role:
- Atrioventricular (AV) Valves (Tricuspid and Mitral/Bicuspid):
- These valves separate the atria from the ventricles.
- Moreover, they open during ventricular diastole (filling), allowing blood to flow from the atria to the ventricles.
- However, they close during ventricular systole, preventing blood from flowing back into the atria.
- Semilunar Valves (Aortic and Pulmonary):
- These valves separate the ventricles from the major arteries (aorta and pulmonary artery).
- They open during ventricular systole, allowing blood to flow into the arteries.
- Thus, they close during ventricular diastole, preventing blood from flowing back into the ventricles.
Key Structures of the Heart
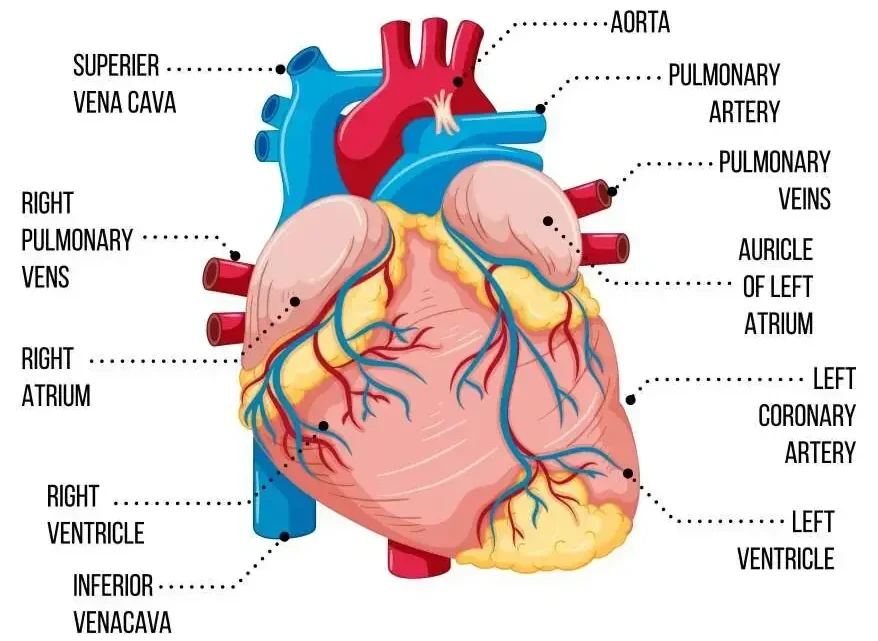
- Four Chambers: Right atrium, right ventricle, left atrium, left ventricle.
- Four Valves: Whereas tricuspid, mitral (bicuspid), pulmonary, and aortic valves.
- Heart Wall Layers: Epicardium, myocardium, and endocardium.
- Major Blood Vessels: Superior and inferior vena cavae, pulmonary arteries and veins, and aorta.
- Pericardium: Thus, the protective sac surrounding the heart.
- Conduction System: Sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers.
How Do the Atria and Ventricles Function Differently
- Atria:
- Act as receiving chambers for blood returning to the heart.
- Basically, the function is to complete ventricular filling by contracting during atrial systole.
- Have thinner walls because they pump blood over a shorter distance into the ventricles.
- Ventricles:
- Act as pumping chambers, propelling blood out of the heart.
- The left heart chamber sends blood with oxygen to the body. The right heart chamber sends blood without oxygen to the lungs.
- Have thicker walls, especially the left ventricle, because they must generate greater pressure to pump blood.
The heart’s real story is detected where its beat and the ECG’s signals come together.
Significance of the Heart’s Electrical Conduction System
- Initiation of Heartbeat:
- The SA node, the heart’s built-in timekeeper, starts the electrical signal. This signal makes the heart beat.
- Coordination of Contractions:
- Also, the conduction system makes sure the atria and ventricles squeeze in a timed way. This makes the heart pump better.
- Regulation of Heart Rate:
- Also, the SA node sets the heart’s pace. The nervous system and hormones can change this pace.
- Also, the SA node sets the heart’s pace. The nervous system and hormones can change this pace.
- ECG Generation:
- The heart’s electrical activity makes an ECG. This test gives helpful information for figuring out health problems.
- The heart’s electrical activity makes an ECG. This test gives helpful information for figuring out health problems.
How Does the Coronary Circulation Support Cardiac Function?
- Oxygen and Nutrient Delivery:
- Also, the heart’s arteries give the heart muscle blood full of oxygen, which it needs to work.
- Waste Removal:
- The heart veins take away used blood and waste from the heart muscle.
- Prevention of Ischemia:
- Hence, adequate coronary circulation prevents ischemia (lack of blood flow) and angina (chest pain). This is also caused by reduced blood supply to the heart muscle.
- Overall Heart Health:
- Additionally, healthy heart arteries are needed to keep your heart strong and stop heart problems.
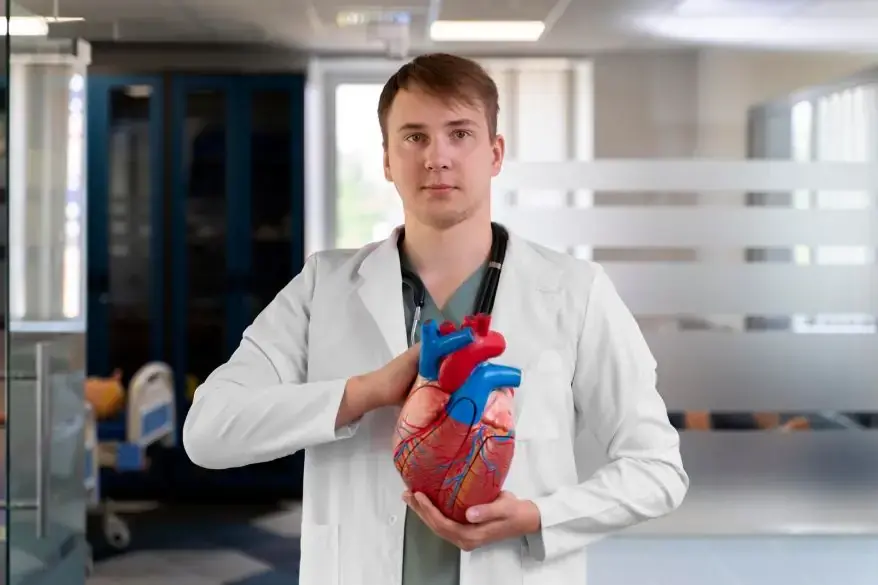
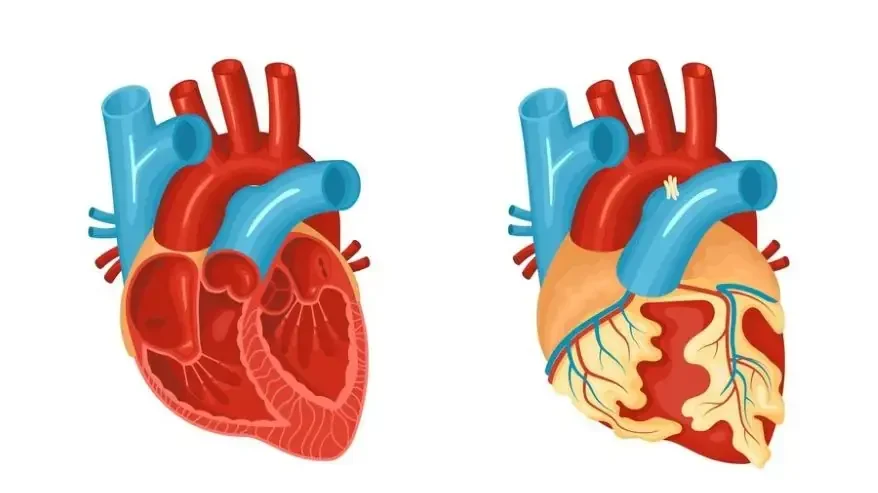
Cardiac Cycle: Anatomy of Heart
To understand the cardiac cycle, you need to grasp the key anatomical features of the heart:
1. Chambers:
- Right Atrium:
- Receives deoxygenated blood from the superior and inferior vena cavae.
- Plays a role in initiating the cardiac cycle via the SA node.
- Right Ventricle:
- Pumps deoxygenated blood to the lungs through the pulmonary arteries.
- Left Atrium:
- Receives oxygenated blood from the pulmonary veins.
- Left Ventricle:
- Pumps oxygenated blood to the body through the aorta.
- Has the thickest walls, crucial for generating high pressure.
2. Valves:
- Atrioventricular (AV) Valves:
- Tricuspid Valve (Right AV): Between the right atrium and ventricle.
- Mitral (Bicuspid) Valve (Left AV): Between the left atrium and ventricle.
- These valves prevent backflow of blood from the ventricles to the atria during systole.
- Semilunar Valves:
- Pulmonary Valve: Between the right ventricle and pulmonary arteries.
- Aortic Valve: Between the left ventricle and the aorta.
- These valves prevent backflow of blood from the arteries to the ventricles during diastole.
3. Heart Wall Layers:
- Myocardium: The muscular layer; its contraction drives the cardiac cycle. The thickness of this layer varies between the atria and ventricles, and within the ventricles themselves.
- Endocardium: The inner lining that comes into contact with blood.
- Epicardium: The outer layer.
4. Major Blood Vessels:
- Vena Cave (Superior and Inferior): Return deoxygenated blood to the right atrium.
- Pulmonary Arteries: Carry deoxygenated blood to the lungs.
- Pulmonary Veins: Carry oxygenated blood from the lungs to the left atrium.
- Aorta: Carries oxygenated blood to the body.
How these structures relate to the Cardiac Cycle:
- The atria act as receiving chambers, and their contraction (atrial systole) completes ventricular filling.
- Ventricles are the pumping chambers, and their contraction also ejects blood into the circulation.
- Valves ensure direct blood flow, crucial for the efficient pumping action of the heart.
- The myocardium is the muscle that contracts and relaxes to push the blood through the heart.
- The blood vessels are the highways for the blood, to and from the heart.
Knowing how these parts fit together and what they do helps you picture and understand the heart’s movement.
Cardiac Cycle: Physiology of the Heart
The heart works through complex systems that let it pump blood well. So here’s an overview of key aspects:

1. Electrical Conduction System:
- Sinoatrial (SA) Node:
- The heart’s natural pacemaker, located in the right atrium.
- Generates electrical impulses that initiate each heartbeat.
- Atrioventricular (AV) Node:
- Delays the electrical impulse, in fact, by allowing the atria to contract before the ventricles.
- Bundle of His:
- Thus, transmits the impulse from the AV node to the ventricles.
- Purkinje Fibers:
- Also, send the signal through the heart in the bottom parts, so they press together at once.
2. Cardiac Cycle:
- Systole (Contraction):
- Atrial systole: Atria contract, pushing blood into the ventricles.
- Thus, ventricular systole: Ventricles contract, pumping blood into the aorta and pulmonary artery.
- Diastole (Relaxation):
- Atria and ventricles relax, allowing them to fill with blood.
- Heart Valves:
- Ensure single-way blood flow.
- Additionally, AV valves (tricuspid and mitral) prevent backflow from ventricles to atria.
- Also, semilunar valves (aortic and pulmonary) prevent backflow from arteries to ventricles.
3. Cardiac Output:
- Heart Rate (HR):
- Number of heartbeats per minute.
- Stroke Volume (SV):
- Moreover, the volume of blood is pumped by the left ventricle with each contraction.
- Cardiac Output (CO):
- Thus, the volume of blood pumped by the heart per minute (CO = HR x SV).
- Hence, the volume of blood pumped by the heart per minute (CO = HR x SV).
- Cardiac output is managed by the autonomic nervous system, also, hormones, and other factors.
4. Regulation of Heart Function:
- Autonomic Nervous System:
- Sympathetic nervous system: Increases HR and contraction.
- Specifically, the anabolic nervous system decreases HR.
- Hormones:
- Epinephrine (adrenaline): Increases HR and contractility.
- Other hormones also affect the heart.
- Frank-Starling Law:
- Additionally, the heart pumps out whatever volume of blood it receives (within physiological limits).
5. Coronary Circulation:
- Thus, the coronary arteries supply the heart muscle with oxygenated blood.
- Moreover, coronary veins drain deoxygenated blood from the heart muscle.
Key Physiological Processes:
- Action Potentials: Electrical signals that trigger muscle contraction.
- Calcium Ions: Moreover, they play a crucial role in muscle contraction.
- Pressure Gradients: Drive blood flow through the heart.
Conclusion
In short, the heart works in a specific order to keep us alive. The atria and ventricles squeeze in time, and there are key times for rest. Also, each part is needed to keep blood moving steadily. Knowing how this cycle works helps us see how the heart works and why heart health matters. Problems with this rhythm, thus it caused by sickness or how we live, can be very bad. We should be aware of and take care of our hearts. Understanding the heart’s beat and its sections helps us see why it is important. Then we can look after it properly.
FAQ’s
1. What is the cardiac cycle?
- A: The heart cycle is everything that happens in the heart from one beat to the next. This includes when the heart chambers squeeze and when they loosen.
2. What is systole?
- A: Systole happens when the heart squeezes and pushes blood out.
3. What is diastole?
- A: Diastole is the relaxation phase of the cardiac cycle, when the heart chambers fill with blood.
References
- Dotter, C. T. (1955). Motion in cardiovascular radiography. Circulation, 12(6), 1034–1042. https://doi.org/10.1161/01.cir.12.6.1034
- Occhetta, E., Corbucci, G., Bortnik, M., Pedrigi, C., Said, S. a. M., Droste, H. T., Hofmann, R., & Marino, P. (2010). Do electrical parameters of the cardiac cycle reflect the corresponding mechanical intervals as the heart rate changes? EP Europace, 12(6), 830–834. https://doi.org/10.1093/europace/euq068
Additionally, to stay updated with the latest developments in STEM research, visit ENTECH Online. Basically, this is our digital magazine for science, technology, engineering, and mathematics. Further, at ENTECH Online, you’ll find a wealth of information.
Disclaimer: We do not intend this blog post to provide professional, technical, or medical advice. Therefore, please consult a health professional before making any changes to your diet or lifestyle. In fact, we only use AI-generated images for illustration and decoration. Their accuracy, quality, and appropriate can differ. So, users should avoid making decisions or assumptions based only on the text and image