Revolutionizing Diabetes Treatment: Oral Insulin Delivery
The International Diabetes Federation has predicted that people with diabetes aged 20 – 79 years rise to 642 million by 2040. Incidentally, 75% of people with diabetes are living in countries with low and medium incomes. Thus, diabetes management becomes more critical for poor countries to develop affordable, effective remedies. The quest for better alternatives has led researchers to explore oral insulin delivery, which mimics the way our body naturally releases insulin from the pancreas. Firstly, there is a need to understand some basics about diabetes for better judgement.
Understanding Diabetes
The Inherent Nature of Disease
Diabetes is a disease that is caused due to malfunctioning of the body’s organs. The health of body organs mainly depends on the genes gifted by the father and mother’s gene banks. The truth is that even the color, size, or shape of a single hair of our body never crosses the limits of our gene source. Broadly, we can make out the nature of our life journey from the history of our father and mother gene resources. The change in life patterns related to eating, physical work, etc., can vary our life journey, but not significantly.
Thus, the disease related to organ failure cannot be cured unless and until we replace it with a healthy and compatible organ. This process is highly cost-intensive and only under the supervision of expert physicians and surgeons it is possible but maybe with a very low success rate. Thus, in the case of diabetes, we can manage it, but we cannot cure it. The claim about diabetic cure and no side effects of the drug due to its herbal source is reaching our drawing room regularly and needs expert scrutiny. The whole life system of the earth is made of chemicals. Thus, the herbal source is not a chemical or harmful chemical is just a marketing gimmick. The entry of any chemical, herbal or non-herbal, which is foreign to the body is bound to generate a reaction.
The oral insulin delivery approach mimics the body’s natural insulin secretion process, offering a significant improvement in patient quality of life. However, significant challenges remain.
The Bioavailability Hurdle
One major obstacle is the low bioavailability of insulin when taken orally. Insulin, a protein, is susceptible to degradation by enzymes in the digestive tract, reducing the amount that reaches the bloodstream. Furthermore, the use of unsuitable carriers can lead to carrier toxicity, posing additional health risks. Researchers are working to overcome these problems by developing novel delivery systems.
Peptide Structure and Enzyme Resistance
Researchers investigated peptides composed of 16 to 20 L-amino acids. They found that peptides offering moderate protection against pepsin (a stomach enzyme) and some protection against trypsin and chymotrypsin (pancreatic enzymes) significantly improved insulin bioavailability. Interestingly, peptides with strong protection against trypsin but no protection against pepsin were less effective. This highlights the complex interplay between peptide structure and enzyme resistance in determining oral insulin delivery success.
In in vitro testing, these insulin-peptide complexes demonstrated remarkable stability against enzyme degradation. The in vivo results were equally encouraging. Oral administration of the insulin-peptide complexes resulted in detectable insulin levels (10-41%) in blood plasma within 30 to 60 minutes. This is a significant step towards a more practical and comfortable diabetes treatment.
The Role of Glucose in the Body
The Importance of Glucose
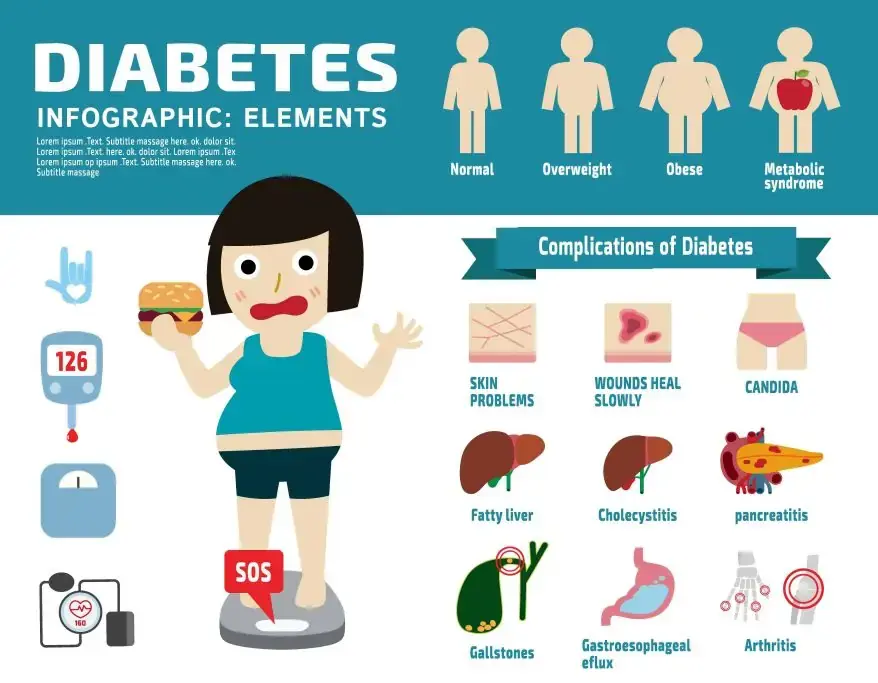
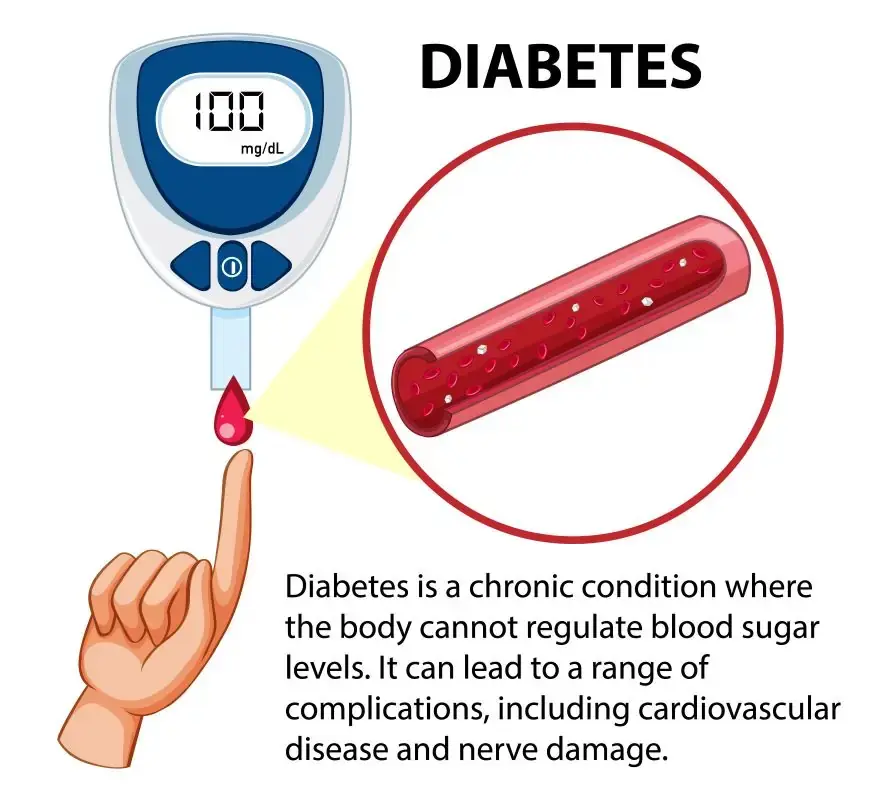
Popularly, diabetes is called a disease of sugar, whereas sugar is a source of life energy that cannot be compromised. Generally, the adult brain uses roughly 120 grams of glucose each day. This shows the importance of glucose in our lives, as our bodies use glucose as a source of energy to carry out different functions. The body prepares glucose from dietary carbohydrates as its primary form of energy. When glucose levels start rising in the blood after a meal, the beta cells of the pancreas secrete insulin. Insulin acts as a key to open the cells to take in glucose from the blood to generate energy to carry out their normal function.
When the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen. The body converts stored glycogen into glucose in case of emergency. Whenever the body’s normal function of glucose management is disturbed, it results in a disease commonly known as diabetes. This disease is characterized by excess sugar in the blood and urine.
In general, diabetes is classified as Type 1 and Type 2. An autoimmune destruction of insulin beta cells in the pancreas causes type 1 diabetes, which doctors control through parenteral administration of insulin. In contrast, type 2 diabetes is characterized by varying degrees of insulin resistance, impaired insulin secretion, and increased glucose production, and doctors generally control it with oral anti-diabetic agents.
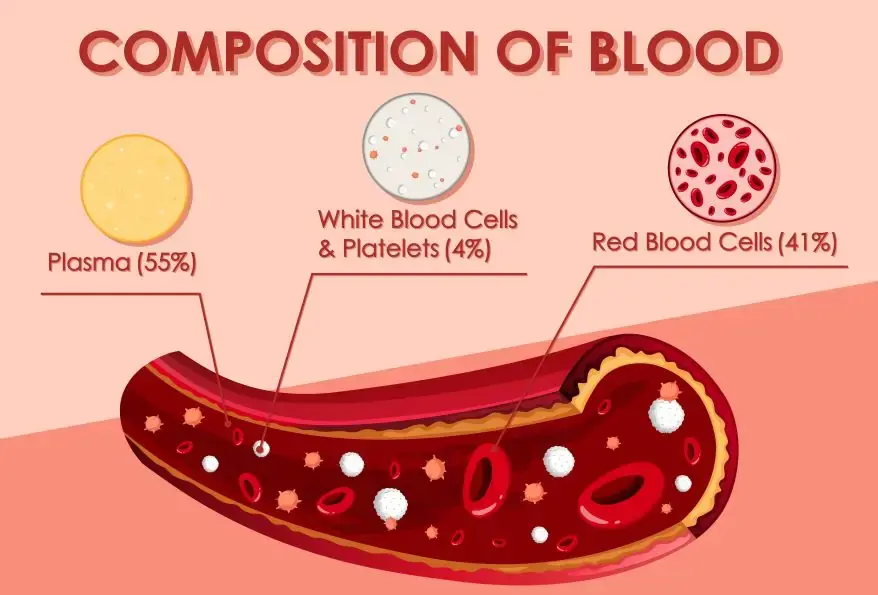
When oral anti-diabetic agents fail to reduce glycemia, doctors treat these patients with insulin. Therefore, doctors administer insulin parenterally as the only effective therapeutic agent for treating diabetes. Insulin, a hormone secreted by all mammals, including humans, plays a crucial role in this process. Hormones are proteins that act as a messenger to control and coordinate different activities of the body.
A Brief History of Diabetes
As around four million people are dying per year due to diabetes, that indicates the need for proper management of the disease is of high importance. The history of diabetes may go back to the evolution of mammals, as all mammals, including humans, produce insulin. However, there was no effective treatment, and people usually died within weeks to months of first showing symptoms.
Ancient India discovered the use of ants for testing diabetes. If ants were attracted to the urine, it signified high sugar levels, and this condition was called Madhumeha. Around the fifth century B.C.E., the people of India and China were aware of the difference between type 1 and type 2 diabetes. Apollonius of Memphis mentioned the term “diabetes” during the third century B.C.E. In 1899, Joseph von Mering and Oskar Minkowski discovered the role of the pancreas in diabetes. Sir Edward Albert Sharpey-Schafer discovered in 1910 that diabetes developed when there was a lack of a particular chemical that the pancreas produced. He named that chemical insulin which means island, as the cells in the islets of Langerhans in the pancreas produce it.
Frederick Banting and Charles Best reversed diabetes in dogs with diabetes by treating it with an extract of pancreatic islet cells from healthy dogs in 1921.
Toronto General Hospital administered the first insulin injection
Generally, this hospital used to keep the children dying from diabetic ketoacidosis in a large ward. Whereas family members helplessly watch their children until they meet with their inevitable death. The hospital followed this routine until 11 January 1922, when Leonard Thompson, a 14-year-old boy, received the first injection of insulin. However, he suffered a severe allergic reaction, leading to the cancellation of further injections. James Collip worked tirelessly for 12 days to improve the ox-pancreas extract, and on 23 January, he administered a second dose. This dose eliminated the glycosuria sign of diabetes without any side effects.
Thus, from this day onwards, people with Type 1 diabetes stop dying. In 1923, Frederick G Banting received the Nobel Prize for the discovery of insulin along with JJR Macleod and shared award money with his colleague Charles H Best. This way, insulin has become an effective drug for the treatment of diabetes mellitus.

The Importance of Insulin
However, calling insulin a drug may be an exaggeration, as the body naturally secretes it to manage its normal function. Thus, one has to take it externally when the body ceases to produce it. Generally, people with type 1 diabetes and some people with type 2 diabetes need to take insulin daily. Any other thing cannot replace insulin.
Occasionally, it appears the body is managing without it, but actually, it keeps on degenerating different organs at a slow pace in its absence. As the body has a natural defense mechanism that keeps it going until it exhausts all its sources. Thus, once the physician advises insulin, it is not good to go for anything else. Not everyone with type 2 diabetes needs insulin; doctors can manage the condition by recommending lifestyle changes and using oral anti-diabetic agents. Available oral anti-diabetic agents include metformin, sulfonylureas, pramlintide, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and glucagon-like peptide 1 (GLP-1) receptor inhibitors.
Oral Insulin Delivery: Future Directions and Potential Impact
Currently, scientists are working on immunotherapy and an artificial pancreas for the better management of type 1 diabetes. However, whichever way is suitable for the particular patient is the prerogative of the expert physician and not any drawing room expert? The basic problem is that the cost of disease management is going out of the reach of common people. And this is the reason that people seek another alternative and compromise their life. This is not the impossible thing, and we can overcome it effortlessly using available technologies.
While these findings are encouraging, further research is necessary to optimize peptide design and improve the consistency of insulin absorption.
Nevertheless, this approach represents a significant advancement in oral insulin delivery. Advantages of using artificial peptides include reduced pain associated with injections and a more physiological approach to delivering this crucial medication. Successful development of this technology would revolutionize diabetes management, offering a less invasive and more convenient treatment option for millions.
Reference
- Adikane, H. V. [WO Patent (Pub. No. WO/2020/026272, 06.02. 2020)] Oral insulin delivery using artificial peptide. (2021d). Indian Journal of Biochemistry and Biophysics. https://doi.org/10.56042/ijbb.v58i5.30338
- Keeling, A. (2009). International Diabetes Federation – the Global Voice for Diabetes. touchREVIEWS in Endocrinology, 05(0), 18. https://doi.org/10.17925/ee.2009.05.00.18
- Perrotti, N., Santoro, D., Genovese, S., Giacco, A., Rivellese, A., & Riccardi, G. (1984). Effect of digestible carbohydrates on glucose control in insulin-dependent diabetic patients. Diabetes Care, 7(4), 354–359. https://doi.org/10.2337/diacare.7.4.354
- Gannon, M. C., & Nuttall, F. Q. (2004). Effect of a High-Protein, Low-Carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes, 53(9), 2375–2382. https://doi.org/10.2337/diabetes.53.9.2375
Additionally, to stay updated with the latest developments in STEM research, visit ENTECH Online. Basically, this is our digital magazine for science, technology, engineering, and mathematics. Furthermore, at ENTECH Online, you’ll find a wealth of information.
Disclaimer: We do not intend this article/blog post to provide professional, technical, or medical advice. Therefore, please consult a healthcare professional before making any changes to your diet or lifestyle. In fact, we only use AI-generated images for illustration and decoration. Their accuracy, quality, and appropriateness can differ. So, users should avoid making decisions or assumptions based only on the text and images.







